Changing Payers After Encounters
Changing Payer Periods Even After Encounters to Re-Bill Correctly
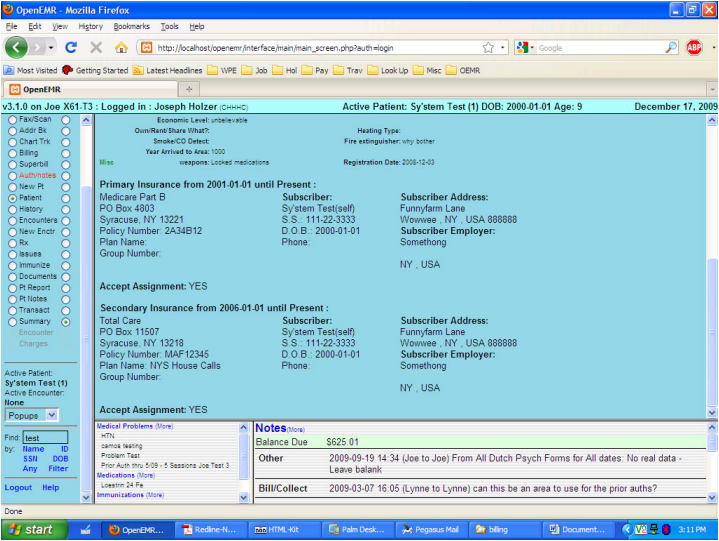
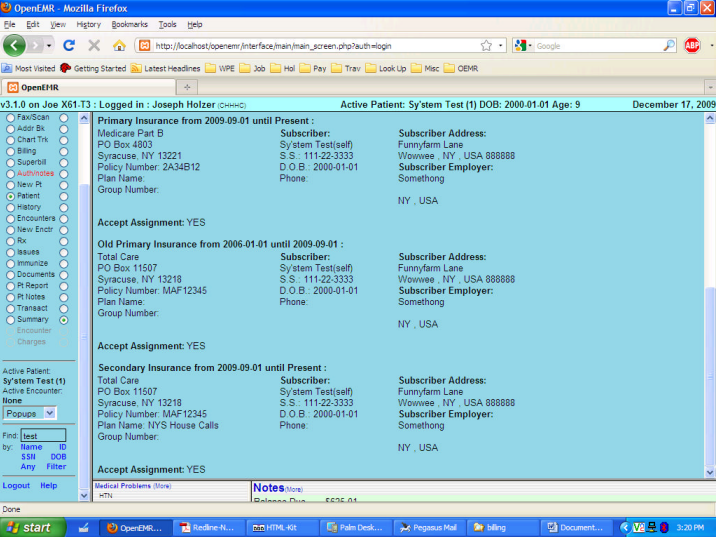
Situation: Patient provided data showing Medicare was primary payer, but Medicare says effective date was later, and secondary payer listed is actually primary. This shows you how to fix that. The screenshot below shows the Patient Demographics as they have been, in the Insurance area at the bottom.
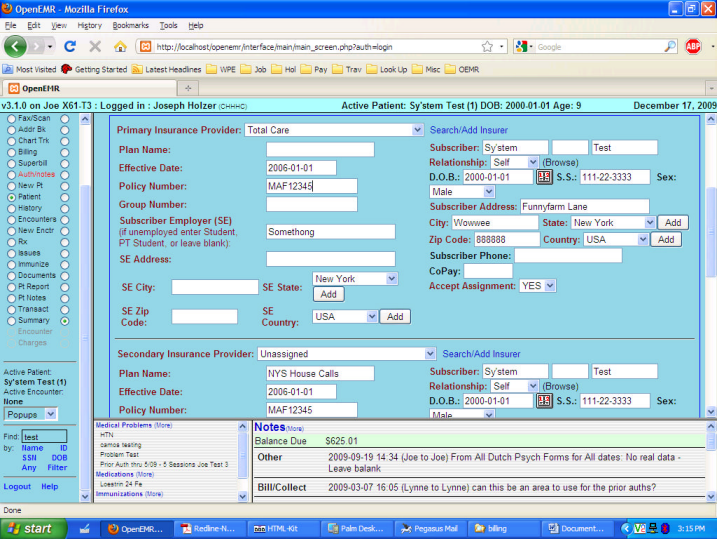
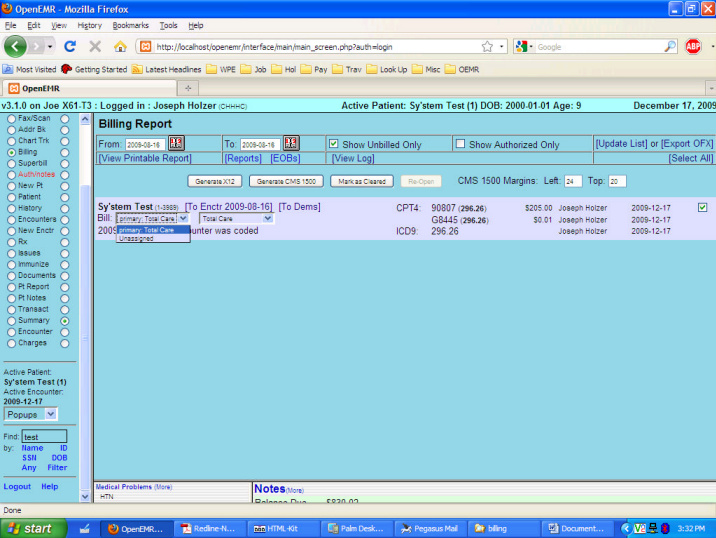
You must click on the (More) at the top of that frame to allow edits of the Insurance settings to correct them to what was actually the case for the earlier visits, with the actual Effective Date if it differs (you can leave the earliest effective date if it does not affect any of your actual encounters, even if the policy was not really in place at that earlier date; OpenEMR only uses the date to determine who is to be billed in what order). Change the Primary to the correct payer (Total Care in this case) and fix any as needed of the correct policy number, plan name, policy holder, etc, with the correct Effective Date. Change the Secondary to Unassigned – you can leave all the rest as- is to save typing later. See the screenshot below for details. If the correct payer name and address data is not yet entered, use the Admin – Practice – Insurance to set that up. Remember to save before leaving the demographics. By changing the effective date, you will change the From / To period shown in bold above the insurance info.
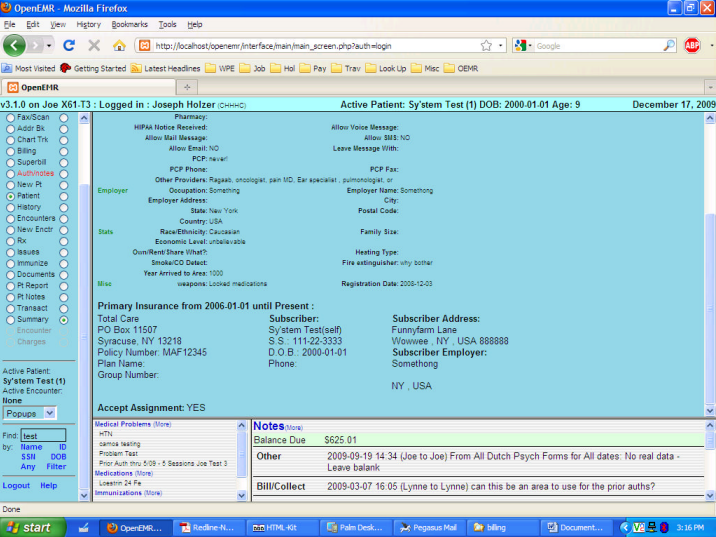
Once you have saved that, you will notice that the Demographics now shows only the single insurer, with its Effective date for the “From” and “Present” as the “To” date, per the screenshot below.
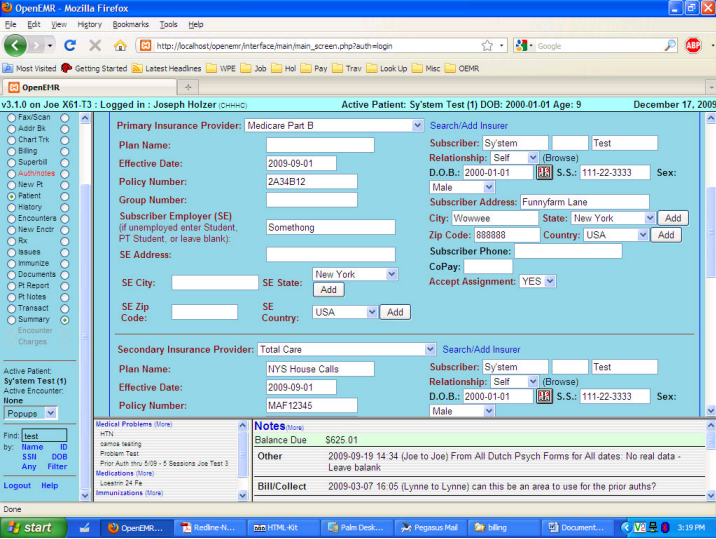
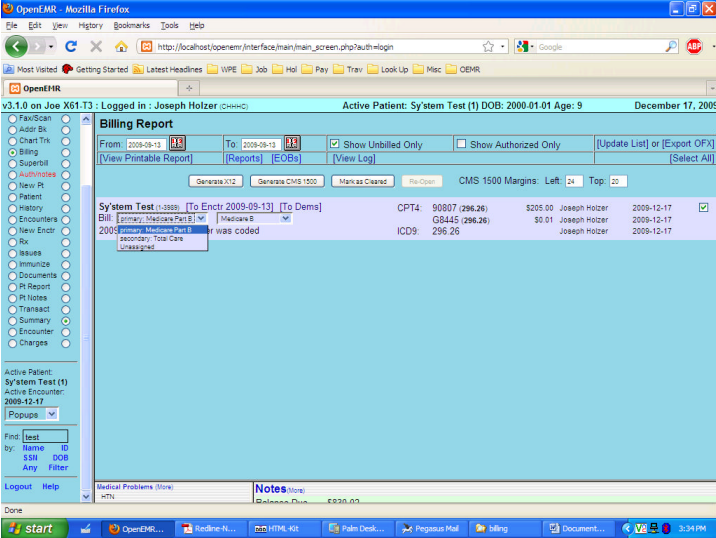
Now again go back to edit the Insurance info by selecting the (More) at the frame top, and click on the Insurance box, then begin to edit per the screenshot below. Note that we again select the previous primary of Medicare, and the previous secondary of Total Care, and again fix any plan names, etc. as needed. Note that the previously left secondary info is still there, even though the “Unassigned” made it sort of invisible to the claims process. This time, though, we will make the Effective Date for the Medicare what it was supposed to be AND we make the effective date for the secondary the same date. That will assure that claims for services before Medicare went into effect will be billed to Total Care, but from the effective date of Medicare, Total Care will only be billed once the primary, Medicare, has been completed in the EOB area (see “Billing” below).
Again, save after you have made the changes, and the first screenshot in Part 2 should reflect the new data at the bottom of Demographics. You will notice it shows different periods for each of the insurance coverages. That data will now be used by OpenEMR, based on service date, to prepare bills. As you can guess, over time you are likely to have multiples of each shown for each patient as they change insurers or plans. You should follow this process any time information must change in the bill in order to be paid properly. So, for example, you must create a new period every time a BCBS policy number changes, etc.
If you had previously billed an encounter, you must first “ReOpen” it. Looking at the screenshot below, once you check the box to the far right, that would be one of the choices if the “Unbilled” had been unchecked, in addition to the X12 and CMS 1500 (which better reflects the reality and is now in the CVS for next release, but your copy may still say “HCFA” – they are the same, merely labeled differently). Had you merely selected the date, without removing the checkmark for the “Unbilled”, your list would not have found the previously billed encounter. And once you have re-opened an encounter, the “Unbilled” must have the checkmark (the default) to display that encounter for billing again. Note that because our service date precedes the effective date for Medicare as Primary, only the Total Care is shown as the default, along with its default X12 Partner in the box to its right. In all cases you will see “Unassigned” as one of the drop-down choices, and if you selected it, any data shown in Demographics under the “Unassigned” would print, but it is meaningless.
If, however, we have an encounter which falls after the effective date which changes who covers what, you can see in the screenshot below the impact that has, which will carry to the bills. When you bill this, the info for both the Primary and Secondary will be shown in the CMS 1500 and X12 outputs. The Secondary bill will also only print once the Primary has been accounted for within the “EOB” section as accessed at the [EOBs] link, or from the “Invoice” section of the Collections Report links column, which you can access from the main left frame “Reports” radio button. The [Reports] link in the Billing module only displays the “Cash Receipts by Provider report. A bunch of changes to the Billing module are anticipated in the next (3.2) release, and this document will be updated then.